64 YEAR OLD MALE WITH DECREASED URINE OUTPUT AND SHORTNESS OF BREATH.
This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
Chief Complaints:
A 64 year old Male patient resident of Nalgonda, who was a RTC Driver 15years back ,came to the opd with chief complaints of :
1) Decreased urine output since 20 days
2) Shortness of breath since 20 days
3) Pedal edema since 20 days.
History of presenting illness:
• 10 years ago he was working as a driver and owned a vegetable shop , for few days he was not feeling well and he visited local hospital , diagnosed as hypertensive , he is on T-Aten-Am 50mg.
• 5years ago,he got injured to his left palm when he was cutting a tree, he had pain,swelling and blackish discoloration,he was then incidentally diagnosed as diabetic and is on medication Tab.Metformin 500 mg.The injury healed.
• 4 years ago he had an injury when he fell from his bike and injured his chest which led to fracture of ribs (5,6,7) left side and punctured his lung leading to hemoptysis.He was in hospital for 1 month and it got settled down.
•30 days back he got injury to his right little toe with a stone , gradually a bleb was formed which spontaneously ruptured with fluid and blood oozing out and developed an ulcer for which he took over the counter medications for about 10 days
It was associated with pain,swelling , low grade on and off fever which relieved with medication.
• Decreased urine output since 20 days , burning micturition.
• He went to a government hospital in nalgonda and was diagnosed as AKI on CKD and was transferred to private hospital 1 for dialysis, there he developed
Shortness of breath grade 2 - grade 3 with orthopnea.
• Bilateral pedal edema which was insidious in onset and gradually progressive upto level of knee.
• Also facial puffiness
He went through dialysis 1
• Because of financial issues he was transferred to hospital 2.
• Presented with ulcer of right foot since 20 days.
Decreased urine output since 20 days with burning micturition
Shortness of breath grade 2 - grade 3 with orthopnea.
Generalised anasarca.
• Complaints of hematuria after foley's catheterization i/v/o low urine output.
• He was dialysed for 4times in hospital 2, after the 1st dialysis he developed rash with itching over abdomen ,axilla and back which was papular and erythematous for which dvl referral was done and diagnosed as drug induced urticaria.
• After 4 dialysis sessions Patient is feeling better comparatively but still has low urine output and sob.
• DIALYSIS 1 - 3/1/22
• DIALYSIS 2- 5/1/22
• DIALYSIS 3- 7/1/22
• DIALYSIS 4- 9/1/22.
PAST HISTORY:
• No similar complaints in the past.
• h/o hypertension since 10 years and is on Tab.ATEN.
• h/o Diabetes mellitus since 5 years and is on Tab.METFORMIN.
• No h/o asthma, tuberculosis , epilepsy , cad.
PERSONAL HISTORY:
Decreased appetite since 3 days.
Mixed diet.
Sleep : adequate, now decreased.
Bowel Movements : Regular.
Bladder: Decreased Urine Output.
No history of allergies.
Alcoholic since 40 years , 90 ml per day ,last binge 25 days back.
Smoking since 40 years, 1 pack per day.
FAMILY HISTORY:
Patients mother has diabetes.
GENERAL EXAMINATION:
The patient is conscious, coherent and cooperative.
He is moderately built and nourished.
PALLOR - absent
Icterus - Absent
Cyanosis - Absent
Clubbing - Absent
Lymphadenopathy - Absent
Pedal oedema - PRESENT ( PITTING TYPE)
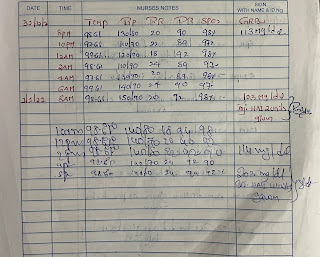
Vitals:
Temperature- afebrile
Pulse rate- 68 beats per minute
Respiratory rate- 22 breaths per minute
B.P- 160/90 mm hg
SpO2- 99% at room air
SYSTEMIC EXAMINATION
Abdomen : Soft and Non tender.
CVS : S1and S2 are heard
No murmurs are heard
Respiratory system:
Dyspnoea- Present
Breath sounds- decreased breath sounds in right and crepitations are heard.
BAE- present
Central nervous system-
Patient was conscious coherent and cooperative.
Speech was normal.
No slurred speech
No meningeal irritation signs
-No abnormality detected.
Gait : Normal.
INVESTIGATIONS:
30-12-21
Ultrasound abdomen.
31-12-21
Hemogram:
2-1-22
4-1-22
6-1-22
8-1-22
ECG.
Diagnosis : AKI ON CKD SECONDARY TO RIGHT LOWER LIMB CELLULITIS WITH HYPERTENSION AND DIABETES.
Treatment:
31/12/2021
IVF.NS OR RL UO+50ml/ hr
INJ Lasix 40mg iv/BD
INJ Piptaz 2.25gm iv / TID
INJ nodosis 500mg po/TID
CAP BioD3 0.2mg po/Od
Mgso4 dressing for R. Lower limb cellulitis
RLL elevation
Monitor vitals
Charting
GRBS 6th hrly
Inj HAI s/c 8am 2pm 8 am.
01/01/2022
Add on
Tab ni cardio 5mg Po/Bd
02/01/2022
Add on
Slat restriction
Fluid restriction
Tab nicardia 10mg
03/01/2022
Add on
Pan 40mg/bd
06/01/2022
Add on
Inj clindamycin 600mg Iv/TDS
8/1/21:
1) Fluid restriction less than 1litre per day.
2) salt restriction less than 2.4 gm per day.
3)tab. Lasix 40 mg po /bd.
4)IVF - uo + 30 ml / hr.
5)inj.HAI s/c acc to sliding scale inf 9154575437.
6) tab . Nodosis 500mg/TID.
7)Cap. Bio d-3 0.25 mg/ od
8)tab.nicardia 10 mg / bid.
9)inj. Pan 40 mg iv /od.
10) Right lower limb elevation.
11)inj.piptaz 2.25 mg iv /tid.
12) inj. clindamycin 600 mg/iv/tid.
Added On
13)onit. Thromboprobe.


































Comments
Post a Comment